The miseducation of immune T cells: how ovarian cancer resists immunotherapy
Immune checkpoint inhibitors (ICI), which help immune T cells identify and kill tumor cells, are most effective in patients who have tumor antigen-specific T cells in circulation. Studies have shown that patients with ovarian cancer do have such tumor-reactive T cells in their blood, indicating a “naturally occurring, antitumor immune response.” So why do only 10-15% of ovarian cancer patients respond favorably to ICI therapy? This was the question former Damon Runyon Clinical Investigator Ronald J. Buckanovich, MD, PhD, and his team at the University of Pittsburgh set out to answer in a recent study.
They suspected the explanation lay in the ovarian tumor microenvironment (TME)—the normal cells, signaling molecules, and blood vessels that surround a tumor. Ovarian cancer patients have a worse prognosis when their TME exhibits desmoplasia, or the formation of fibrous, scar-like tissue around the tumor, as if it were a wound instead of a cancer. Because desmoplasia helps tumors resist chemotherapy, the team reasoned it might help them resist immune cell attack as well.
As one might expect, desmoplasia relies on the same stem cells that are responsible for wound healing and other regenerative processes. Found throughout the body, these are called mesenchymal stem cells (MSCs), and they have the capacity to develop into many different types of cells, including the fibroblasts that constitute scar tissue and desmoplasia. MSCs can therefore play both sides, so to speak, helping the body heal from wounds or helping tumors resist therapy. Which side they choose, according to the team’s findings, depends on their degree of “cancer education”—in other words, where they happen to grow. If MSCs grow up in the same tissue as the tumor, the tumor microenvironment can reprogram them into cancer-associated MSCs (CA-MSCs), effectively recruiting them to the cancer’s side.
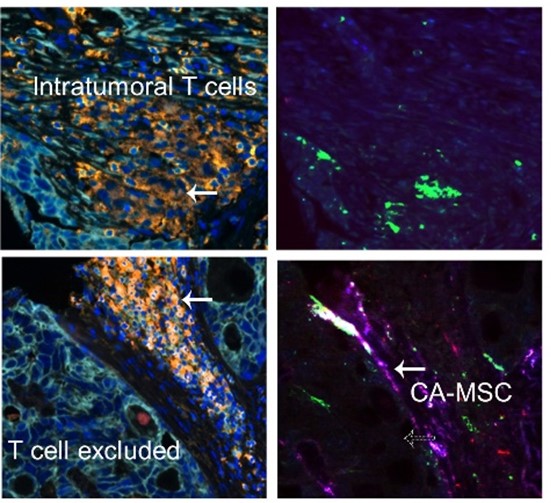
Once ovarian MSCs become CA-MSCs, they develop into fibroblasts (i.e., promote desmoplasia) through a pathway known as the Hedgehog signaling pathway, which tells stem cells what kind of cells to become. (This pathway is crucial for embryonic development, and earned its name because fruit fly larvae missing the key signaling molecule develop abnormally stubby bodies, like hedgehogs.) The resulting scar-like tissue around the tumor keeps immune cells out, protecting the tumor from ICI therapy.
Having unraveled this complex tale of MSC allegiance and sabotage, the team put the data to exciting use. By inhibiting the Hedgehog signaling pathway, the team was able to reduce the number of ovarian CA-MSCs and reverse the desmoplastic response. This, in turn, allowed T cells to infiltrate the tissue, ultimately rendering the tumor sensitive to ICI therapy. With their findings, Dr. Buckanovich and his team have unlocked an important mechanism of treatment resistance and revealed a promising new target for ICI-resistant ovarian cancer therapy.
This research was published in Science Advances.
