Early immunotherapy drug shows new promise against glioblastoma in mice
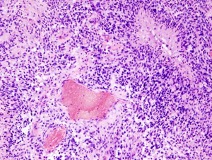
Glioblastoma, the most common and aggressive form of brain cancer, is notoriously difficult to treat. Once arisen, the tumor rapidly invades healthy brain tissue, making removal by surgery nearly impossible and chemotherapy or radiation therapy success short-lived. Even immunotherapy drugs, increasingly relied upon when first lines of treatment fail, have proven ineffective, leaving glioblastoma patients with very few options. But this may change soon.
A new study from former Damon Runyon Fellows Susan M. Kaech, PhD, and Thomas H. Mann, PhD, at the Salk Institute for Biological Studies shows that an immunotherapy drug called anti-CTLA-4 significantly improved survival rates in mice with glioblastoma. Anti-CTLA-4 belongs to a class of drugs known as immune checkpoint inhibitors: it blocks a protein called CTLA-4, which, if not blocked, binds and “turns off” immune T cells. Anti-CTLA-4 was actually the first immune checkpoint inhibitor approved for the treatment of cancer, but it was soon eclipsed by another checkpoint inhibitor, anti-PD-1, which was less toxic and became more popular both in research and clinical use. After seeing that anti-PD-1 did not work against glioblastoma, however, the team wondered if anti-CTLA-4 could prevail instead.
To their surprise, the researchers found that anti-CTLA-4 not only succeeded in shrinking the tumors but did so by recruiting two other overlooked cancer-fighting agents: microglia, the brain’s resident immune cells, which patrol for tissue damage but have not been known to attack tumors, and CD4+ T cells, referred to as “helper T cells” because, unlike CD8+ T cells, they do not kill cancer cells directly. But together, it turns out, microglia and helper T cells are more powerful than they seem. Treatment with anti-CTLA-4 caused CD4+ cells to secrete a protein called interferon gamma, which alerted the microglia to the presence of glioblastoma cells and prompted phagocytosis, or “eating,” of the tumor cells. In turn, as the microglia “ate” the tumor cells, they presented tumor antigens on their surface to keep the CD4+ cells active, creating a feedback loop that lasted until the tumor cells were eliminated.
“There are currently no effective treatments for glioblastoma—a diagnosis today is basically a death sentence,” Dr. Kaech told the Salk Institute. “We're extremely excited to find an immunotherapy regimen that uses the mouse’s own immune cells to fight the brain cancer and leads to considerable shrinkage, and in some cases elimination, of the tumor.”
The next step will be to test if this tumor-killing circuit can be activated against human glioblastoma cells.
This research was published in Immunity.
